If you are suffering from serious tooth pain that is caused by either serious tooth decay or a bad infection, you may be in need of root canal treatment.
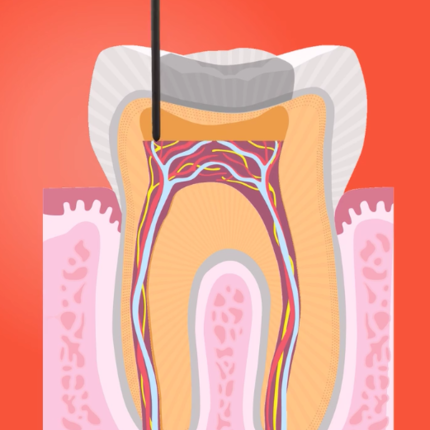
A root canal is a dental treatment that repairs your damaged tooth, saving it from having to be removed. The procedure is called a root canal because it involves cleaning out the internal canals of your tooth that extend into the tooth’s root.
While root canals have an outdated reputation for being painful, the truth is that modern dental anaesthetics have advanced significantly, making most root canal procedures totally pain free. In fact, living with an infected or decaying tooth is much more painful than a quick root canal procedure that’s no more painful than a filling placement.
Signs That You Need A Root Canal
What are the signs that you may need a root canal to repair a damaged tooth? How do you know if you need a root canal treatment?
At the core of your teeth is a soft pulp known as “dental pulp.” This pulp sits in the main body of your teeth (known as a “crown”), and extends all the way down to the root of your teeth. This pulp is home to blood vessels, nerves, and connective tissue that are vulnerable to infection. Once a tooth becomes damaged, bacteria seep into the cracked tooth and enter the pulp.
If the damaged tooth is not repaired promptly, these bacteria that enter the pulp can cause an infection that can kill the dental pulp, lead to bone loss, and potentially cause the loss of the entire tooth.
Just because you have tooth pain doesn’t mean you are absolutely in need of a root canal. But there are several major signs of what may be an infection serious enough to require treatment.
Some of these signs that you may need a root canal include:
- A hole, chip, or crack in your tooth
- Significant toothache pain while chewing, or serious tooth pain when putting pressure on the tooth
- Tenderness or swelling of the gum area surrounding the tooth
- Additional swelling around your face and/or neck
- An abscess or lesion formed on the gum area surrounding the tooth, similar to a small pimple or blister
- Extreme sensitivity or pain in your tooth when exposed to either hot or cold food/drink that lasts beyond the removal of the hot or cold food/drink
- Darkening or discoloration of the tooth
What Is Root Canal Treatment?
The root canal procedure, also known as root canal therapy, is all about cleaning out the infected pulp and removing damaged nerves. This sounds intimidating, but the nerves at the roots of your teeth don’t serve any purpose other than detecting temperature.
A root canal is performed by a general dentist or a specialized endodontist. Endodontists have received four or more years of additional special training specifically to diagnose tooth pain and to perfect the art of root canals, making them known as specialists in saving teeth.
These root canals typically take one or two visits to the dentist to complete. Especially difficult causes can require additional appointments.
Steps in a Root Canal Procedure
Step 1 – The first step of a root canal procedure is to perform dental X-rays that scope out the degree of the damage to the dental pulp. The X-rays also let your dentist see the exact shape of your tooth’s root canals and allow them to see the location of the infection and whether or not there is significant damage incurred to the surrounding bone.
Step 2 – The second step of the procedure involves a local anesthetic. This anesthetic is issued to the area surrounding the tooth, numbing the area to prevent you from feeling any pain throughout the root canal process. In many cases, the nerve will be dead and won’t actually require an anesthetic, but the dentist will still provide you with a local anesthetic to make you more relaxed, and to avoid the chance of any pain whatsoever.
Step 3 – In order to ensure the area around the tooth stays completely dry, your dentist will place a rubber sheet called a dental dam or rubber dam around the tooth. This keeps the tooth clean and saliva free.
Step 4 – Next, the main part of the procedure begins: your dentist will create an opening into your tooth. A hole is made into the crown of your tooth, which will provide an access point to the tooth’s interior. This process is totally painless. Once the hole is made, your dentist will remove the decayed pulp from your tooth’s root. This process is performed by a series of root canal files that enter through the hole and scrub the sides of the canal. Any excess debris or bacteria in the tooth will also be removed.
Step 5 – If there was an infection in your tooth, your dentist may medicate the opening in your tooth. In some cases, your dentist may need to leave your tooth open in order for additional bacteria to drain out. Depending on the dentist, they may only place a temporary filling in your tooth to cap it off until your next visit.
Step 6 – Either in your next visit, or immediately after your procedure, depending on the severity of the infection, your tooth will be fully sealed off. Your dentist will replace the removed dental pulp with a sealant paste and a rubber compound. Then, you will receive a filling to protect the inside of your teeth from saliva.
Step 7 – As most teeth needing root canals will have experienced significant damage, a final step is needed to restore the tooth. Typically, the crown of your tooth will be replaced with an artificial crown that matches the exact colour and shade of your teeth. This crown will protect the tooth from future infection.
To learn more about the warning signs of needing root canal treatment, contact Vitality today.
What to do next?
The Vitality team are always happy to answer any questions regarding tooth pain and how to know if you need root canal treatment. If you have any concerns and have signs you need root canal, please book an initial consultation with one of our clinical dentists today.